You Can Pass the AMC and Still Struggle in Australia. Here’s Why.
Read time: 6 minutes
I have watched capable doctors pass the AMC and expect the pressure to ease.
It rarely does.
What changes is not the difficulty, but the type of difficulty.
The Australian Medical Council (AMC) Clinical Examination is designed, appropriately, to assess whether a candidate meets the standard of a new Australian medical graduate about to start internship.
It tests clinical reasoning, communication, and safety within time-limited, simulated encounters.
What it does not—and cannot—fully assess is what comes next.
Once independent practice begins, particularly in community and private settings, the pressures shift sharply.
Many of the most consequential challenges are not clinical in the narrow sense, but regulatory, interpersonal, medico-legal, and systemic.
This is not a criticism of the exam.
It is a description of reality.
Below, I outline seven domains of Australian medical practice that consistently challenge IMGs after they pass—often in ways they did not anticipate.
Passing the AMC is an entry point, not a finish line.

1. Patient pressure to prescribe
In day-to-day practice, doctors face frequent requests for medications with dependence or regulatory risk: opioids, benzodiazepines, stimulants, and medicinal cannabis.¹
While pharmacology is examined, the legal and relational complexity of refusing, tapering, or negotiating these requests is largely learned in practice.
Indemnity data show medication-related issues account for a significant proportion of GP complaints, particularly around drugs of dependence.
The difficulty is not knowing what to prescribe, but managing conflict, safety, and documentation when saying no.
2. Complaints, notifications, and litigation exposure
Across a 30-year medical career, the majority of doctors will receive at least one complaint or notification.²
Most do not result in loss of registration, but the emotional and professional impact is substantial.³
Let me be clear: only a small minority of notifications—around 2%—result in loss of registration.
As stated by Associate Professor Kudzai Kanhutu, a board member of AHPRA, deregistration cases involve severe, often egregious conduct—a point she reinforced at the 2025 IMG Conference hosted by the Australian Medical Council.
Image A — Complaint received (ZOOM-In to read)
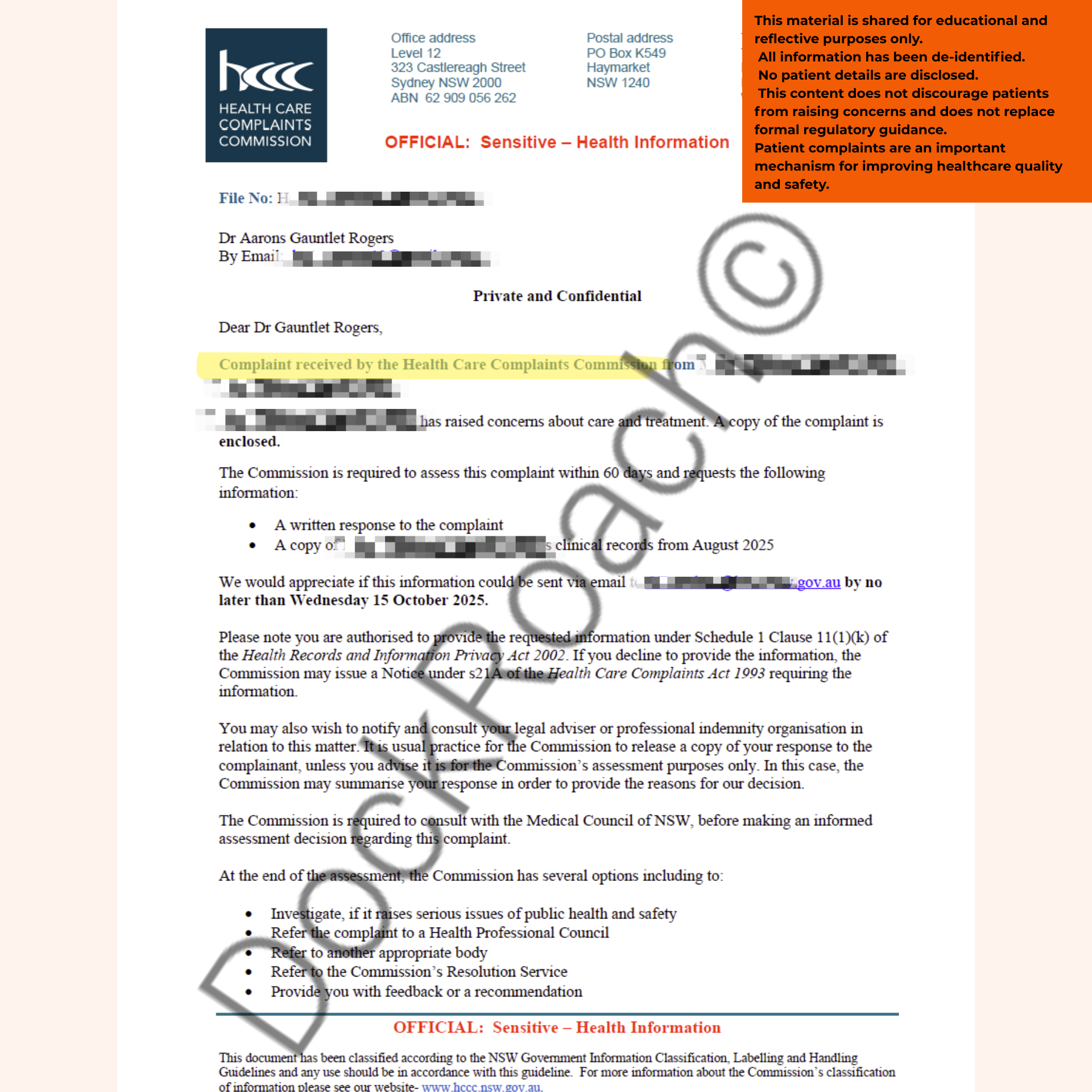
This letter did not arrive because I failed the AMC.
It arrived because I was practising medicine in Australia.