Part 2: Structure in Clinical Tasks – How Top-Scorers Do It in the AMC Clinical Exam
Part 2 of the AMC Clinical Exam Scenario Series
Read time: 5 minutes
Top scorers don’t ‘wing it’ when the bell rings — they’ve already rehearsed the opening act.
Today, I’m going to show you how top-scoring candidates lock in a clear clinical plan in the final moments before the bell — and carry that clarity through:
-
Task 1: Focused history
-
Task 2: Physical exam request & interpretation from the examiner
-
Task 3: Diagnosis & initial management
We’ll apply this step-by-step to Q51: Headache — so you can copy the thinking, not just the theory.
If you missed the previous step, catch up here before reading on.
Why this matters?
When the bell rings (Assessment Time), you don’t want to “find your medicine.” You want to execute it.
Clinical clarity (using structure/ frameworks) in the first minute sets the tone for the entire 8-minute station.
Why most candidates struggle for their exam?
-
They start talking before framing their differentials
-
They ask generic history questions that don’t change task 3
-
They miss red flags, then run out of time explaining a vague diagnosis
Structure beats memory—especially under pressure.
In coaching over a hundred candidates, I’ve found that staying structured requires more than just practice — it demands a deeper understanding that can be trained.
To keep this simple and clear, I break a top-scorer’s profile into four core dimensions.
One of these — Clinical Medicine Application — is about answering clinical tasks with precision. When this is balanced with the other three dimensions, your role-play execution becomes flawless. No anxiety. No panic. Just calm, confident performance.
Most candidates, however, allow anxiety and intrusive thoughts to interfere — breaking their flow and crippling their clinical execution.
Scroll down to see the big picture.
The 4 Dimensions You’ll Need (big picture)

-
Mental Readiness & Professional Conduct (Mindset & Composure)
-
Clinical Medicine Application (Knowledge in Action)
-
Communication & Interpersonal Command (Connection & Projection)
-
Time & Flow Management Under Exam Conditions (Pacing & Control)
Clinical Medicine Application — the ability to apply your knowledge in the Australian context with precision.
It’s not about dumping every fact you know, but about recognising what matters most in the station and adapting that knowledge in real time.
The 7Q–3D Flow (your clinical snap-frame)
Use this fast mental pass to turn the stem + tasks into a clinical plan.
7Q: The Seven Clinical Reading Questions (applied to Q51)
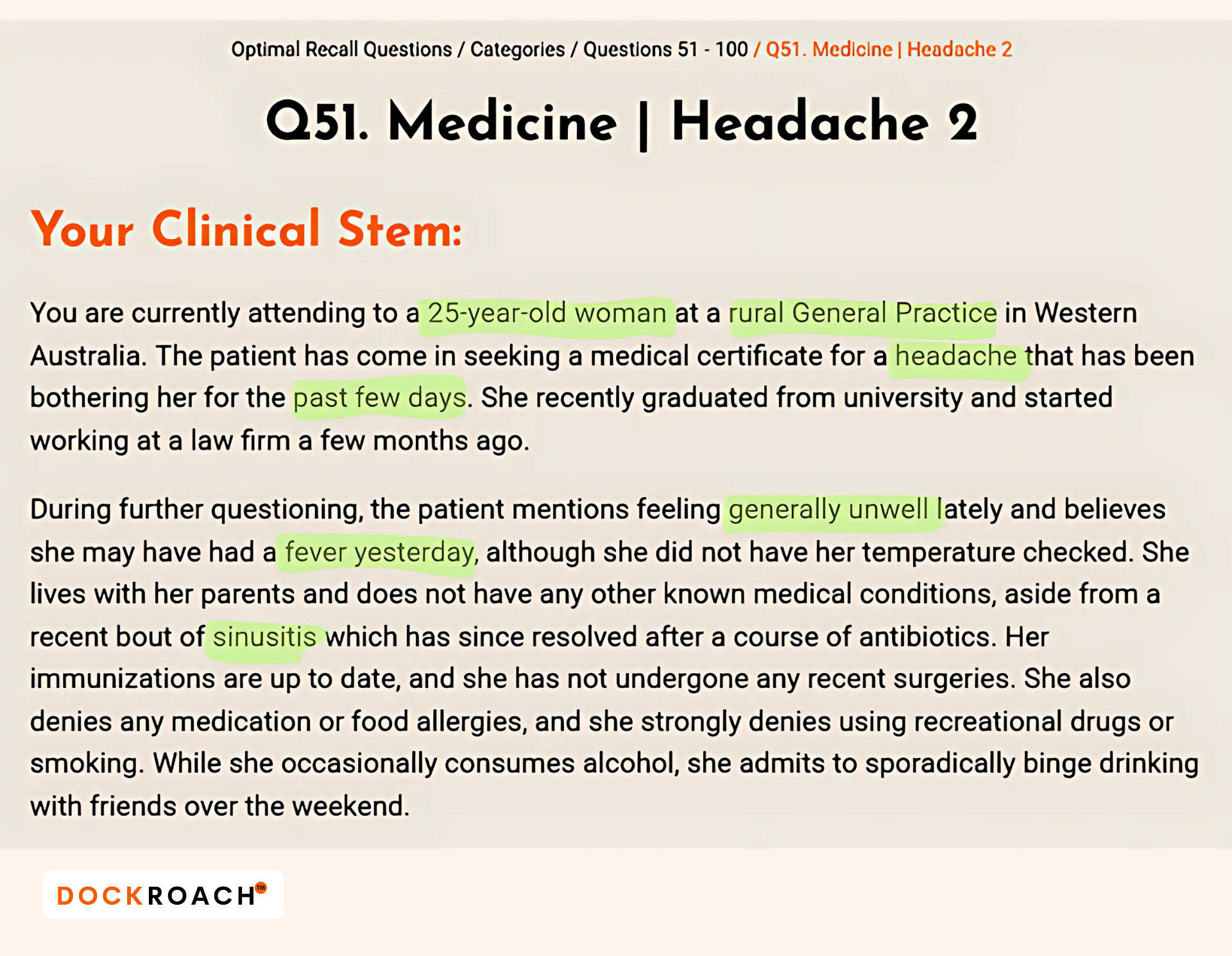
-
WHERE is it? Rural GP Clinic
-
WHO is it? 25‑year‑old woman
-
WHY present? Headache, fever, generally unwell; recent sinusitis
-
WHEN onset? Past few days
-
WHAT subject? Medicine
-
WHAT stage? New/acute presentation
-
WHAT differentials? (build them with 3D below)
3D: Differential Formulation in 3 Simple Steps (1 goal)
Goal: Hold ~7 DDx in order of risk → likelihood → impact on management.
-
D1 — Likely: Migraine, tension headache, post‑infectious headache/viral illness.
-
D2 — Red‑flag set: Meningitis, encephalitis, SAH, intracranial mass.
-
D3 — Less likely by age/demographics (but consider): Cervical spondylosis, malignancy, temporal ateritis; use a global sweep (e.g., your VITAMIN‑A/D/E/K or preferred systems mnemonic) to avoid blind spots.
How to structure Task 1 (History) so Task 3 becomes easy
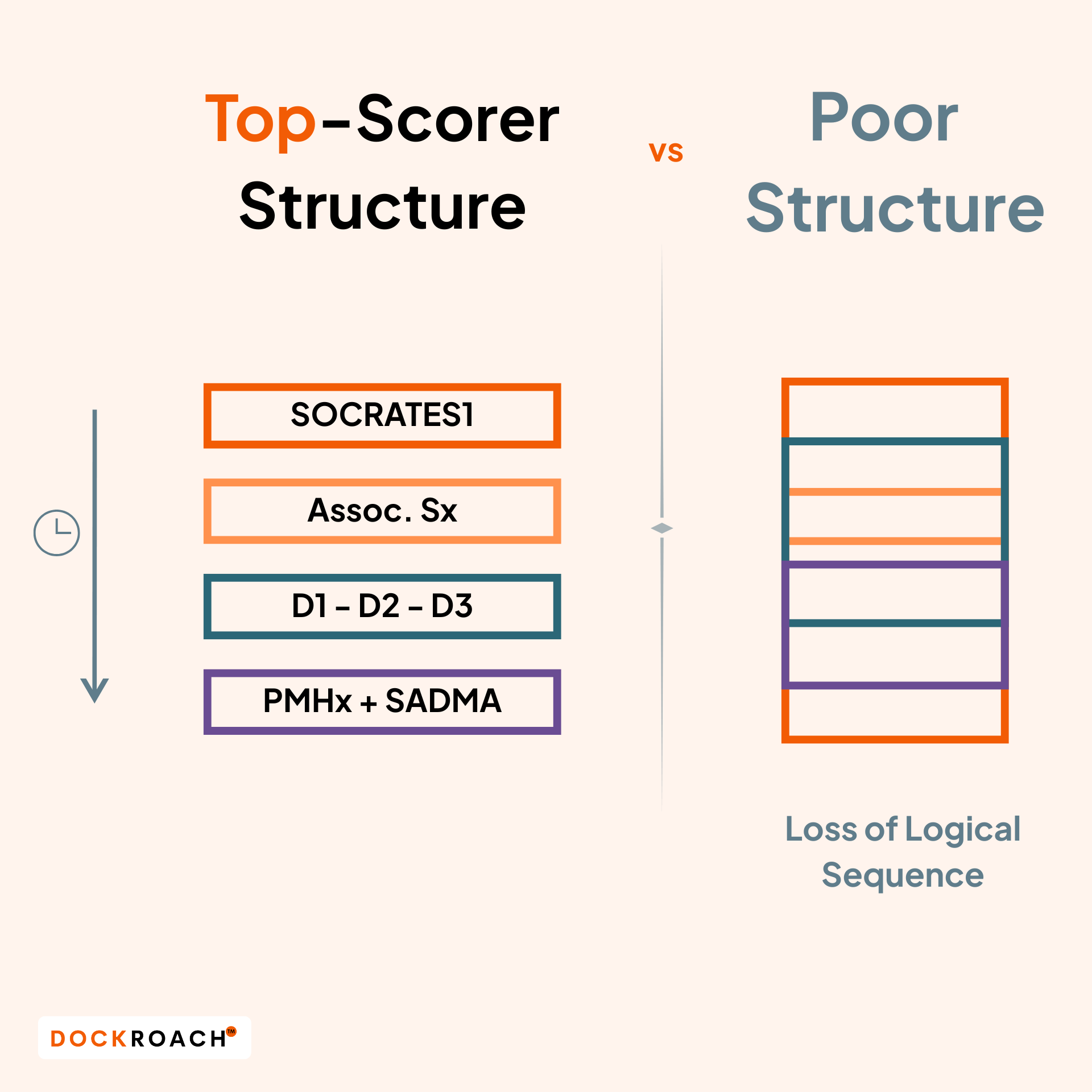
When your 8-minute station begins, stick to these steps without compromise. Then practice them in role plays — over and over — until they feel natural and you can nail them every time.
-
Chief complaint & symptom inquiry:
For headache/pain, use SOCRATES1 + associated symptoms (photophobia, neck stiffness, nausea, rash, neuro deficits).
Refer to the stem for SADMA/past history; don’t re‑ask what’s already given—acknowledge it and move. -
Targeted DDx questions:
-
Meningitis/encephalitis: fever, neck stiffness, rash, photophobia, altered mental state.
-
SAH: “worst headache of life,” thunderclap onset, exertional trigger, meningism, focal neuro signs.
-
Migraine: unilateral, pulsatile, aura, nausea/vomiting, sensory sensitivity, prior episodes.
-
Tension: band‑like, stress, posture, non‑progressive, no red flags.
-
-
Complete only what adds value: brief PMHx, focused meds/allergies (SADMA: confirm from stem), HEADSS if relevant, family history where it changes risk.
Task 1 Outcome: By minute 3–4, you’ve either ruled in/out red flags.
Coaching tip: Follow these rules without compromise — avoid double-barrelled questions, and keep every question in clear, simple English so the patient (and examiner) understands exactly what you mean.
Map your minutes (so medicine lands cleanly)
There’s no on‑screen timer—top candidates train their internal clock with role‑plays.
- Task 1 – Focused history (≈3–4 min unless a prompt dictates):
We've covered this above. - Task 2 – Examination request/interpretation from examiner (≈2 min):
Systematically ask for the relevant exam for your top DDx; state what positive/negative findings you’re seeking and briefly why.
Already part of the DockRoach AMC Clinical Accelerator?
Unlock the systematic approach to Task 2 — including professional sample dialogues you can put into practice today.
Click here to jump right in. -
Task 3 – Dx + initial management (≈2 min):
-
Diagnosis explanation (≈30 sec), plain English.
-
Initial management + safety‑net + follow‑up (reserve more time); check understanding as you go.
-
Coaching tip: If a task has a fixed (prompt) time, use the entire allocation before moving on — you won’t be allowed to start the next task until the time is up.
I’ve watched so many capable candidates stumble here — not because they didn’t know the medicine, but because their sequence fell apart under exam pressure.
Once they practiced the 7Q–3D flow and mapped minutes, their performance felt calm, professional, and precise.
“In the heat of the actual exam, you will not rise to the occasion—you will fall to the level of your training.”
- Adapted from James Clear, Atomic Habits
If you put Q51 through the 7Q–3D right now, where does your plan feel shaky — your history taking, your flow, or your time split?
Want help turning this into automatic execution?
AMC Clinical Accelerator gives you 100 structured scenarios like Q51, with built‑in stem analysis, task decoding, and performance frameworks—so you can run 8‑minute stations with clarity, precision, and calm.
Get started here.
Coming up: Part 3 — Advanced Communication with Time Control. You’ll see exactly how top-scorers close Task 3 in Q51, even when the clock is against them.
That’s all for today. See you in a fortnight.